Pulmonology
- Homepage
- >
- Disease-related malnutrition
- >
- Pulmonology
Therapeutic areas of disease-related malnutrition
- Cancers – Oncology
- Respiratory diseases – Pulmonology
- Stomach and intestinal diseases – Gastroenterology
- Age-related degenerative disorders – Elderly

Disease-related malnutrition is present in a wide range of diseases. The problem is known worldwide, affecting about 20 million patients with the cost of 120 billion Euros in the European Union countries.1 In patients with COPD, disease-related malnutrition is the undernourishment developed due to the presence of the primary disease. In total, 25-40% of these patients exhibit weight loss, with 25% of them having moderate to severe malnutrition and 35% showing a severe disease with a reduced fat free mass index. 2
Patients with COPD are often in a state of marked undernutrition called pulmonary cachexia. Typical metabolic changes associated with the development of this cachectic state are an increased release of pro-inflammatory cytokines, as well as an overactivity of the sympathetic nervous system. Both these changes promote catabolic processes leading to skeletal muscle and fat mass wasting by stimulating lipid utilization and skeletal muscle protein breakdown, while energy intake decreases and energy expenditure increases.3
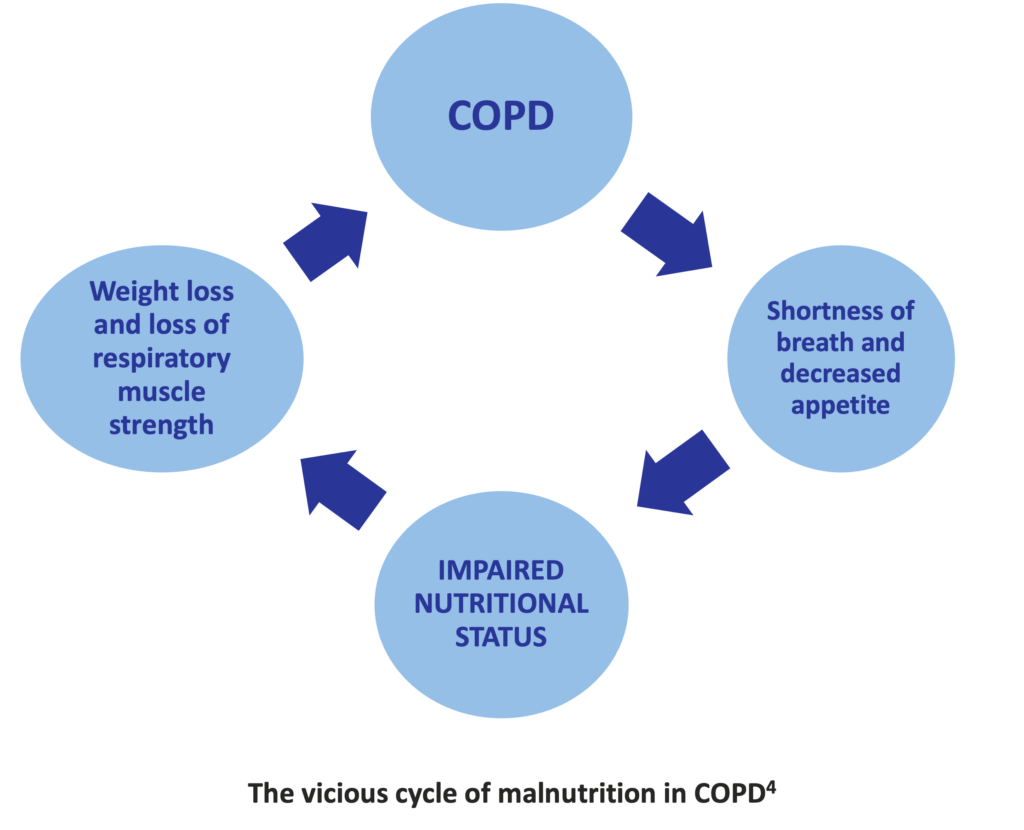
Individuals with COPD often feel anxiety or depression. Both of these feelings can cause decreased appetite. It has been estimated that as many as 50% of patients diagnosed with COPD have clinical depression at some point. Patient’s moods are often affected by the impact their disease has on their lives. These can be changes in the workplace and at home. And there can be changes even in the ability to take care of oneself. Thus, for many patients with COPD, weight loss can become a vicious cycle. The less they eat, the less they feel like eating. 4
Besides decreased appetite, early satiety, dyspnea, fatigue during eating, and social isolation are also factors contributing to the development of malnutrition in COPD patients.
Decreased body weight has been identified as a factor for higher risk of acute exacerbations, lower exercise tolerance, increased risk for hospitalization, reduced quality of life, and poor prognosis in patients with COPD.2
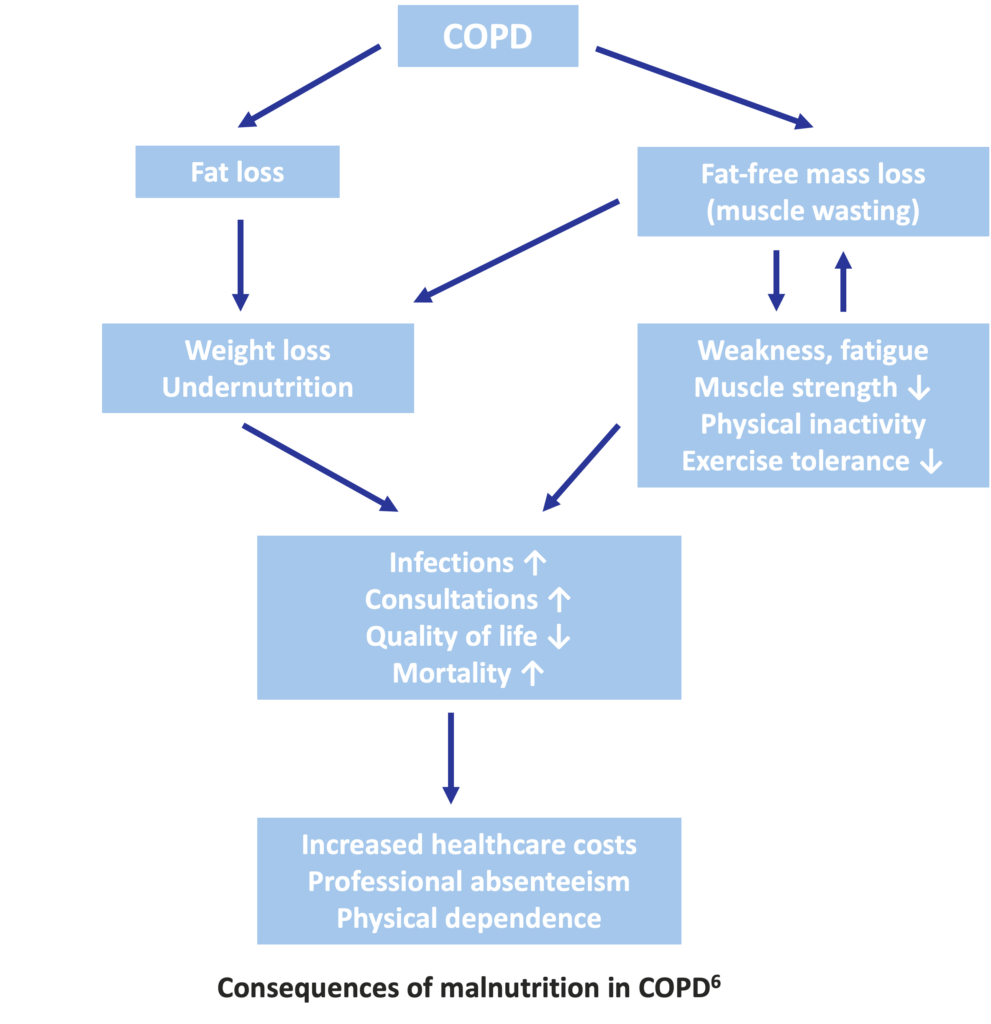
Dyspnea and inflammation increase the energy expenditure and induce decreased food intake and anorexia. These conditions together with insulin resistance and the hypoxia associated with anemia lead to undernutrition characterized by muscle wasting and fat loss. These in turn result in weakness, fatigue, reduced muscle strength, physical inactivity, and reduced exercise tolerance, that are all increased by muscle wasting. The consequences of undernutrition are the increased risk of infections, increased number of medical consultations, impaired quality of life, and poor survival. This unfavourable clinical outcome has economic consequences, such as increased healthcare costs, absence from work, and physical dependence. 6
Getting the right amount of nutrients is crucial for preventing weight loss and muscle wasting to help keep up strength, and to overcome weakness and tiredness. It also helps keep the immune system healthy in order to avoid complications, infections and, ultimately, to recover more quickly.
Nutritional supplement therapies may not only improve undernutrition in COPD patients, but also provide various beneficial effects such as prevention of the progression and exacerbation of the disease, and suppression of the inflammation. 2
The main source of nutrients is normally food. However, for COPD patients suffering from disease-related malnutrition, a healthy diet is often not enough. Since the nutritional demand is increased but appetite is reduced, patients need nutritional supplements that contain high energy in low volume, so even a little quantity significantly boosts the nutritional intake. Specially formulated nutritional products are available for patients to stay well-nourished and fight disease more effectively. They come in all tastes and formats, catering for everyone’s needs.
References:
- Freijer K. et al. The economic costs of disease related malnutrition. Clin Nutr 2013;32:136-41.
- Itoh M. et al. Undernutrition in patients with COPD and its treatment. Nutrients 2013;5:1316-35.
- Müller TD. et al. Ghrelin and its potential in the treatment of eating/wasting disorders and cachexia. J Cachexia Sarcopenia Muscle 2010;1:159-67.
- http://www.copdbfrg.org/, accessed on 6th May 2015
- Dourado VZ. et al. Systemic manifestations in chronic onstructive pulmonary disease. J Bras Pneumol 2006;32:161-71.
- Samaras N. et al. Pulmonary rehabilitation: the reference therapy for undernourished patients with chronic obstructive pulmonary disease.
Biomed Res Int 2014;2014:248420. - Efthimiou J. et al. Effect of carbohydrate rich versus fat rich loads on gas exchange and walking performance in patients with
chronic obstructive lung disease. Thorax 1992;47:451-6. - Kuo C-D. et al. The effects of high-fat and high-carbohydrate diet loads on gas exchange and ventilation in COPD patients and normal subjects.
Chest 1993;104:189-96. - Broekhuizen et al. Polyunsaturated fatty acids improve exercise capacity in chronic obstructive pulmonary disease. Thorax 2005;60:376-82.