Oncology
- Homepage
- >
- Disease-related malnutrition
- >
- Oncology
Therapeutic areas of disease-related malnutrition
- Cancers – Oncology
- Respiratory diseases – Pulmonology
- Stomach and intestinal diseases – Gastroenterology
- Age-related degenerative disorders – Elderly

Disease-related malnutrition is present in a wide range of diseases. The problem is known worldwide, affecting about 20 million patients with the cost of 120 billion Euros in the European Union countries.1 Cancer-related malnutrition is the type of malnutrition triggered by the malignant disease. Cachexia is a complex metabolic syndrome with underlying illness and characterized by loss of muscle with or without loss of fat mass.2 Cancer cachexia is defined as general physical wasting and malnutrition associated with cancer. More than 30% of cancer patients die due to cachexia, while more than 50% die with cachexia being present.3
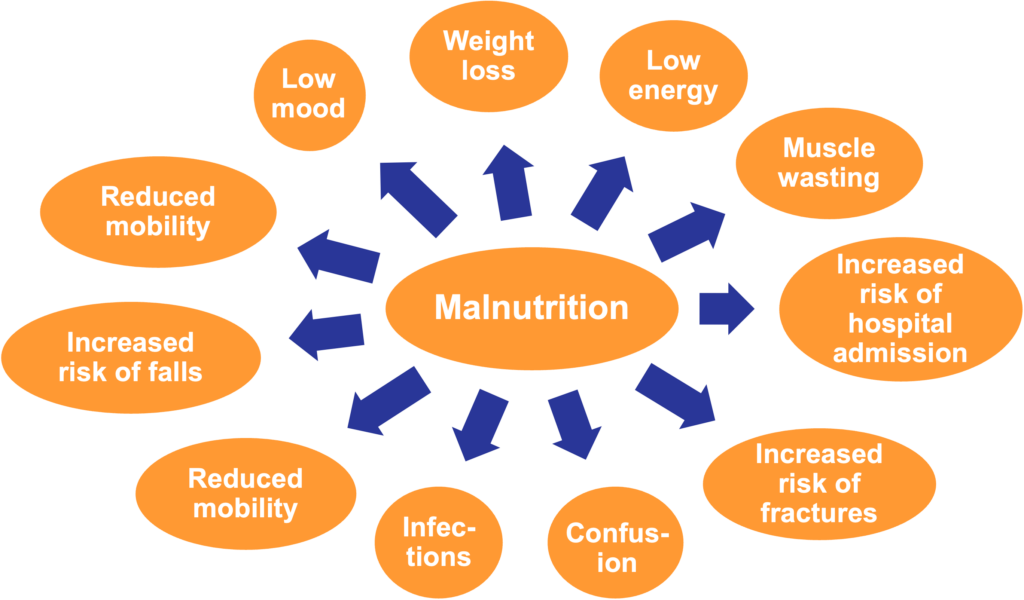
Weight loss / cachexia is a major distress for cancer patients, partly because muscle wasting makes the disease visible. Weight loss is negatively correlated to treatment toxicities, response rate, quality of life and overall survival in cancer patients.4-7 Malnutrition is also an independent predictive factor of early discontinuation of anticancer treatment, which in turn is correlated to poorer results in curative or adjuvant setting.8
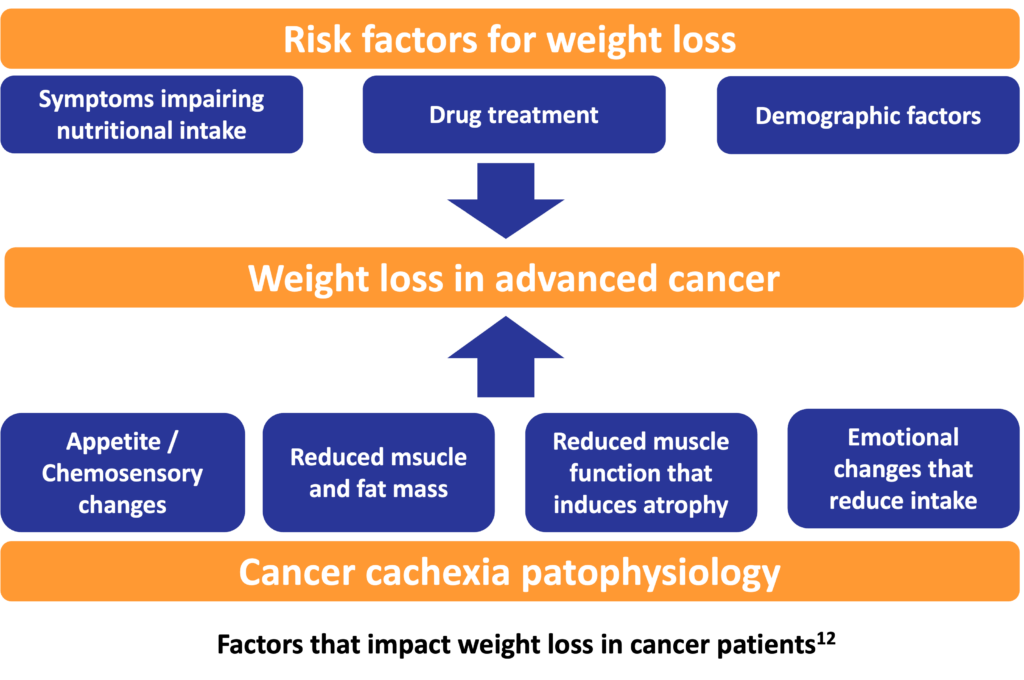
By population prevalence, cancer-related cachexia is one of the most frequent cachexia subtypes.3 Weight loss seen in cancer patients is understood to be driven in a varying degree by low food intake. Low food intake may be the result of a wide variety of symptoms directly or indirectly limiting oral intake. Direct limiting factors among others are anorexia, swallowing difficulties, alterations in taste and smell, while indirect limiting factors include pain and fatigue. A variety of metabolic and endocrine changes, and activation of catabolic pathways account for some of the weight loss that is typically greater than could be expected for the level of food intake.9 Malnutrition and cachexia are common findings in cancer patients, and they become more evident with tumor growth and metastases. The mechanisms by which they are sustained involve damage caused by the primary tumor or by anticancer therapies (surgery, chemotherapy, radiotherapy). Meal-related neural or hormonal signals and humoral signals related to body fat or energy storage and the interaction of these signals with the brain play a pathogenetic role10
Anti-tumor therapies such as surgery, chemotherapy and radiotherapy also have an impact on the nutritional status. Surgery itself can reduce food consumption and increase nutritional requirements. Surgical interventions in the oral cavity, to the tongue, salivary glands, and olfactory nerve lead to loss of taste and smell, which in turn cause reduced food intake and thus nutritional decline. Chemotherapy can affect nutrient uptake and cause metabolic abnormalities, such as hyperglycemia, hypercalcemia, and micronutrient deficiency. Nutritional deficits have specific adverse effects on immune competence. When this is combined with immunocompromised state due to cytotoxic agents, the effect is often doubled. Radiation therapy to the head and neck is associated with anorexia, esophagitis, dryness of the mouth, nausea, vomiting, swallowing difficulties, sore throat, and alterations in taste and smell, all of which can significantly reduce food intake and negatively impact nutritional status. Irradiation of the abdomen or pelvic area may cause acute diarrhea, anorexia, nausea, vomiting, abdominal pain, enteritis and colitis, leading to nutritional deficits.11
Getting the right amount of nutrients is crucial for preventing weight loss and muscle wasting which helps keep up strength, overcome weakness and tiredness. It also helps keep the immune system healthy in order to avoid complications, infections and, ultimately, to recover more quickly.
Nutritional support, addressing the specific needs of cancer patients, is required to help improve prognosis, and reduce the consequences of cancer-related nutritional decline.13
How can we help?
The main source of nutrients is normally food. However, for patients suffering from cancer-related malnutrition, a healthy diet is often not enough. Since the nutritional demand is increased but appetite is reduced, patients need nutritional supplements that contain high energy in low volume, so even a little quantity significantly boosts the nutritional intake. Specially formulated nutritional products are available for patients to stay well-nourished and fight disease more effectively. They come in all tastes and formats, catering for everyone’s needs.
References:
- Freijer K. et al. The economic costs of disease related malnutrition. Clin Nutr 2013;32:136-41.
- Hyltander A. et al. Elevated energy expenditure in cancer patients with solid tumours. Eur J Cancer 1991;27:9-15.
- von Haehling S. and Anker SD. Cachexia as a major underestimated and unmet medical need: facts and numbers. J Cachexia Sarcopenia Muscle 2010;1:1-5.
- Aapro M. et al. Early recognition of malnutrition and cachexia in the cancer patients: a position paper of a European School of Oncology Task Force.
Ann Oncol 2014;25:1492-9. - Andreyev HJ. et al. Why do patients with weight loss have a worse outcome when undergoing chemotherapy for gastrointestinal malignancies?
Eur J Cancer 1998;34:503-9. - Ross PJ. et al. Do patients with weight loss have a worse outcome when undergoing chemotherapy for lung cancers? Br J Cancer 2004;90:1905-11.
- Bachmann J. et al. Cachexia worsens prognosis in patients with resectable pancreatic cancer. J Gastrointest Surg 2008;12:1193-201.
- Kim JW. et al. The early discontinuation of palliative chemotherapy in older patients with cancer. Support Cancer Care 2014;22:773-81.
- Blum D. et al. Cancer cachexia: A systematic literature review of items and domains associated with involuntary weight loss in cancer.
Crit Rev Oncol Hematol 2011;80:114-44. - Nicolini A. et al. Malnutrition, anorexia and cachexia in cancer patients: A mini-review on pathogenesis and treatment.
Biomed Pharmacother 2013;67:807-17. - van Cutsem E. and Arends J. The causes and consequences of cancer-related malnutrition. Eur J Oncol Nurs 2005;9(Suppl 2):S51-63.
- Solheim TS. et al. Weight loss, appetite loss and food intake in cancer patients with cancer cachexia: Three peas in a pod?
– analysis from a multicenter cross-sectional study. Acta Oncol 2014;53:539-46. - Klement J. and Kämmerer U. Is there a role for carbohydrate restriction in the treatment and prevention of cancer? Nutr Metab 2011;8:75.