MediDrink Platinum
- Homepage
- >
- For Healthcare Professionals
- >
- MediDrink Platinum
AGING
Aging is the combined totality of physiological changes that take place in the human body leading to the decreased function of different systems, with negative effects on food intake, health, and quality of life in the elderly (Amarya et al 2015, Shock MW. 2015).
Aging is the combined totality of physiological changes that take place in the human body leading to senescence, the decline of biological functions, and of the ability to adapt to metabolic stress. In humans, the physiological developments are normally accompanied by psychological and behavioral changes, and other changes, involving social and economic factors, also occur. The biological-physiological aspects of aging include both the basic biological factors that underlie aging and the general health status. Since the probability of death increases rapidly with advancing age, changes must clearly occur in the individual which make him more and more vulnerable to disease. For example, a young adult may rapidly recover from pneumonia, whereas an elderly person may die. Physiologists have found that the performance of many organs such as the heart, kidneys, brain, or lungs, show a gradual decline over the life span. Part of this decline is due to a loss of cells from these organs, with consequent reduction in the reserve capacities of the individual. Furthermore, the cells remaining in the elderly individual may not perform as well as those in the young. Certain cellular enzymes may be less active, and thus more time may be required to carry out chemical reactions. Ultimately, the cell may even die (Shock MW. 2015).
Aging and the cardiovascular system
Diseases of the heart are the single largest cause of death above the age of 65. Thus, with increasing age, the heart becomes more vulnerable to disease. Even in the absence of detectable disease, the heart undergoes deleterious changes with advancing age. Structural changes include a gradual loss of muscle fibers with an infiltration of fat and connective tissue. Performance of the heart shows a gradual reduction with advancing age. The amount of blood pumped by the heart diminishes by about 50% between the ages of 20 and 90 years, though there are marked individual differences in the effects of age. Under resting conditions, the heart rate does not change significantly with age. During each beat, however, the muscle fibers of the heart do not contract as rapidly in the old as in the young. This reduction in power, or rate of work, is due to the age-associated reduction in the activities of certain cellular enzymes that produce the energy required for muscular contraction. Despite these changes, the heart, in the absence of disease, is still able to meet the demands placed upon it. In response to physical exercise, it can increase its rate to double or triple the amount of blood pumped each minute, although the maximum possible output falls, and the reserve capacity of the heart diminishes with age (Shock MW. 2015).
In general, blood vessels become less elastic with advancing age. There is a progressive thickening of the walls of larger blood vessels with an increase in connective tissue. The connective tissue itself becomes stiffer with increasing age. This occurs because of the formation of crosslinks both within the molecules of collagen, and between adjacent collagen fibers. These changes in blood vessels occur even in the absence of the deposits on the arterial wall characteristic of atherosclerosis, which interfere with blood flow through the arteries. The gradual loss of elasticity increases resistance to the flow of blood so that blood pressure may increase. This in turn increases the work that the heart must do to maintain the flow of blood. While both systolic and diastolic blood pressures increase with age, the rate of systolic increase exceeds that of diastolic, thus the pulse pressure widens. The increase in pressure stops in the 8th decade of life, and there may even be a slight decline in pressure in extremely old age (Shock MW. 2015).
Aging and the gastrointestinal system
Loss of teeth and improperly fitting dentures may unconsciously change eating patterns because of difficulty with chewing, leading to the intake of a soft, low-fiber diet without important fresh fruits and vegetables. There are some documented gastrointestinal changes in the elderly that can affect their food intake, for example, changes in peristaltic activity of the esophagus, which may result in a delay in esophageal emptying. Widespread nutritional deficiencies are also associated with bacterial contamination of the small bowel. It was found that 17 of 24 malnourished patients had bacterial contamination of the small bowel. There was a significant improvement in the nutritional status of elderly patients after treatment of bacterial contamination with antibiotics. Other gastrointestinal changes occur with age and may affect food intake. For example, greater satiation after a meal and a delay in gastric emptying have been observed in older people (Amarya et al 2015).
Aging and the renal and genitourinary system
In addition to gastrointestinal physiological changes, renal function declines with age. There is a decrease in kidney mass, blood flow, glomerular rate (10% decrement per decade after the age of 30 years), and the elasticity, muscle tone, and capacity of the bladder. Severity can vary, but most cases are mild or moderate in older people, do not cause symptoms, and do not progress to kidney failure. Renal impairment may also affect vitamin D metabolism and result in a reduction of vitamin D levels, which contributes to osteoporosis in the elderly (Amarya et al 2015).
Aging and the nervous system and cognition
With advancing age, risks for cognitive decline increase, affecting the independence and quality of life. Insufficient intake of selected vitamins or certain metabolic disorders may affect cognitive processes by disrupting the nutrient-dependent processes within the body that are associated with the management of energy in neurons, which can subsequently affect synaptic plasticity or the ability to encode new memories. The earliest signs of mild cognitive impairment or pre-Alzheimer’s disease are decreases in the ability to prepare food, forgetting to eat, and inability to access food, which can further impair oral intake (Amarya et al 2015).
Aging and the immune system
The immune defense system is adversely affected by the aging process, and there is strong evidence that a poorly functioning immune system can contribute to decreased disease resistance and reduced life expectancy in the elderly. Elderly people are more likely to die of infections than young adults, and malnutrition is related to an increased risk of sepsis in the elderly. Infections of all kinds increase the metabolic rate, making it more difficult for older persons to eat enough to keep up with energy demands (Amarya et al 2015).
Aging and social and psychological factors
Although not having many close friends contributes to poor health in many older adults, those who also feel lonely face even greater health risks. It is difficult to change some of the already established food habits, carried over from childhood. Food habits are influenced by several factors such as family, education, occupation, economic status, lifestyle, and cultural norms. Factors that have a negative influence on the health and nutrition of the elderly are lack of family support in times of need (because of the widely prevalent nuclear family system), feeling of not being wanted, economic constraints, lack of value system among the members in the family, stressful conditions leading to tensions, and loneliness leading to disinterestedness in living and eating (Amarya et al 2015).
Aging and sensory functions
After the age of 70, sense organs may also show a reduction in sensitivity. The incidence of gross sensory impairments, of which many are the results of disease processes, increases with age. One survey conducted in the US classified 25.9 / 1,000 persons aged 65–74 as blind, in contrast to 1.3 / 1,000 aged 20–44 years. In the age group 65–74, 54.7 / 1,000 persons were classified as functionally deaf, compared with 5.0 / 1,000 in the age range 25–34 years (Shock MW. 2015).
The effect of aging on the sense of smell has not been precisely determined because this sense is extremely difficult to assess quantitatively. In addition, smoking and exposure to occupational odors and noxious substances in the air influence sensitivity to smells (Shock MW. 2015).
There may be a progressive loss in the number of taste buds per papilla on the tongue. The remaining taste buds, which detect primarily bitter or sour tastes, show a relative increase with aging. Impaired appetite is often associated with a reduction in taste and smell, which occurs in up to 50% of elderly people (Amarya et al 2015).
Besides a decline in visual acuity during aging, there is also reduction in the size of the pupil with age. Consequently, vision in older people can be significantly improved by an increase in the level of illumination. Aging also brings about a reduction in the ability to change the focus of the eye for viewing near and far objects. This change in vision is related to a gradual increase in rigidity of the lens of the eye that takes place primarily between the ages of 10 and 55 years. After age 55 there is little further change. The sensitivity of the eye under conditions of low illumination is less in the old than in the young – “night vision” is reduced. Sensitivity to glare is also greater in the old than in the young. The incidence of diseases of the eye, such as glaucoma and cataracts, also increases with age (Shock MW. 2015).
Hearing does not change much with age for tones of frequencies usually encountered in daily life. Above the age of 50, however, there is a gradual reduction in the ability to perceive tones at higher frequencies. Few persons over the age of 65 can hear tones with a frequency of 10,000 Hz. This loss of perception of high frequencies interferes with identifying individuals by their voices and with understanding conversation in a group but does not ordinarily represent a serious limitation to the individual in daily life. Listening habits and intellectual level play an important role in determining the ability to understand speech, so that there is often a disparity between measurements of pure tone thresholds and ability to perceive speech (Shock MW. 2015).
Sensitivity to pain is difficult to evaluate quantitatively under controlled laboratory conditions. There is some evidence that it diminishes slightly after the age of 70 (Shock MW. 2015).
Aging and the musculoskeletal system
With aging, the bones gradually lose calcium. As a result, they become more fragile and are more likely to break, even with minor falls. Healing of fractures is also slower in the old than in the young. The incidence of osteoporosis also increases with age occurring more frequently in women after menopause than in men and being especially evident in the spinal column. The mobility of joints diminishes with age and the incidence of arthritis increases. The capacity to perform muscular work diminishes progressively in the elderly. Muscle strength diminishes, however, the reduction in strength is less in muscles that continue to be used throughout adult life than in those that are not. Thus, a part of the reduction in muscle strength may be an atrophy of disuse. Maximum work capacity is also reduced in the elderly, largely because of the inability to deliver enough oxygen to the working muscles. In the young, the need for oxygen is met for the most part by increasing the heart rate. Under conditions of maximum work, young adults can increase their heart rate to over 200 beats per minute, while the elderly to only about 150 per minute. In addition, the transfer of oxygen from the lungs to the blood is reduced in the elderly under conditions of strenuous exercise. With less than maximum exercise, there is a greater increase in blood pressure, heart rate, and respiration in the old than in the young. Thus, a given workload induces a greater physiological stress in the old than in the young. Furthermore, recovery of blood pressure, heart rate, and respiration to resting values takes longer in the old (Shock MW. 2015).
Bones become less dense partly because they contain less calcium that gives bones strength. The amount of calcium decreases because the body absorbs less calcium from foods. Also, levels of vitamin D that helps the body use calcium, decrease slightly. Certain bones are weakened more than others. Those most affected include the end of the femur at the hip, the ends of the arm bones at the wrist, and the vertebrae. Changes in vertebrae at the top of the spine cause the head to tip forward, compressing the throat. As a result, swallowing is more difficult, and choking is more likely. The vertebrae become less dense and the discs between them lose fluid and become thinner, making the spine shorter. The cartilage that lines the joints tends to thin, partly because of the wear and tear of years of movement. The surfaces of a joint may not slide over each other as well as they used to, and the joint may be slightly more susceptible to injury. Damage to the cartilage due to lifelong use of joints or repeated injury often leads to osteoarthritis, which is one of the most common disorders of later life. Ligaments binding joints together, and tendons binding muscle to bone, tend to become less elastic, making joints feel tight or stiff. These tissues also weaken. Thus, most people become less flexible. Ligaments tend to tear more easily, and when they tear, they heal more slowly (Stefanacci RG. 2022).
There is a general slowing of responses in the elderly. Reflexes become slightly more sluggish and the speed of conduction of impulses in nerves is slightly slowed. Old people require more time to respond to the appearance of a light than do the young. The slowing with age is greater in situations where a decision must be made (Shock MW. 2015).
Aging and the respiratory system
Vital capacity diminishes with age, as does the total volume of air that can be contained in the lungs. In contrast, the amount of air that cannot be expelled from the lung, increases. These changes in respiratory mechanisms are primarily a reflection of the increased stiffness of the bony cage of the chest and the decreased strength of the muscles that move the chest during respiration. Although with age there is a slight reduction in the amount of oxygen that can be moved from the air to the blood in the lungs, the reduction becomes apparent only when large amounts of oxygen are required, as during strenuous exercise. It is believed that a primary factor in the impairment of oxygen transfer in the lungs of elderly subjects is the lack of appropriate adjustment of the blood flow to the air sacs in the lung (Shock MW. 2015).
Aging and metabolism
Basal metabolism decreases with age. According to cross-sectional data of 358 female and 155 male subjects, resting metabolic rate decreases yearly by 8.7 KJ/day in women and by 30.7 kJ/day in men (Luhrmann et al 2010).
In the elderly, the sensitivity of the pancreas is reduced, thus, a higher level of blood sugar is required to stimulate it to action. As a result, one characteristic of aging is a reduction in the rate of removal of excess sugar from the blood (Shock MW. 2015).
When the acidity of the blood is increased to the same extent in old and young subjects, it returns to normal within 6–8 hours in the young; in the elderly 18–24 hours are required (Shock MW. 2015).
The body’s physiological mechanisms for adjusting to changes in environmental temperature are less adequate in the old than in the young. Consequently, older people may prefer more uniform and slightly higher temperatures than the young. High temperatures are also more hazardous to the elderly. The incidence of heat prostration in hot weather increases with age (Shock MW. 2015).
CHRONIC CONDITIONS IN ELDERLIES
Chronic conditions, such as age-related cognitive decline, osteoarthritis, age-related macular degeneration, diabetes, and osteoporosis are common in elderlies. Numerous people may be affected by more than one condition, leading to therapeutic hardships, complications, decreased quality of life, and poorer disease outcomes (Ornstein et al. 2013, Droogsma et al. 2013, Zhang & Jordan. 2010, Rudnicka et al. 2015, Lee et al. 2013).
Aging is the combined totality of physiological changes that take place in the human body leading to senescence, the decline of biological functions, and of the ability to adapt to metabolic stress. Basal metabolism decreases with age, the pancreas becomes less sensitive, and a higher blood sugar level is required to stimulate it to action. Changes in the gastrointestinal system (e.g. changes in the peristaltic activity, decrease of the number of taste buds) can affect the food intake in old people. With increasing age, the heart becomes more vulnerable to disease, renal function declines, vital capacity of the lungs diminishes, the immune system becomes adversely affected, the risk for cognitive impairment increases, the capacity to perform muscular work diminishes, bones become less dense, cartilages tend to thin and get damaged, visual acuity declines, and there is a gradual reduction in the ability to perceive tones at higher frequencies. In summary, numerous bodily functions decline with aging which have a negative effect on the health and quality of life of the elderly (National Academy on an Aging Society. 1999).
More elderlies with chronic conditions are limited in their daily activities by their condition (National Academy on an Aging Society. 1999)
Moreover, elderlies are more prone to having multiple chronic conditions. According to a cross-sectional study of 148 practices with 667,379 active patients, multimorbidity increased steeply with age, levelling off at age 80. Overall, 45.2% of patients had more than one chronic illness (Ornstein et al. 2013).
Multimorbidity increases steeply with age (Ornstein et al. 2013).
Cognitive impairment, Alzheimer’s disease
The number of people with dementia is anticipated to double every 20 years. Despite different inclusion criteria, several meta-analyses and nationwide surveys have yielded roughly similar age-specific prevalence of Alzheimer’s disease, which is a multifactorial neurodegenerative disorder of older adults, across regions. The age-specific prevalence of Alzheimer’s disease almost doubles every 5 years after age 65. Among developed nations, approximately 1 in 10 older people (>65 years) is affected by some degree of dementia, whereas more than one third of very old people (>85 years) may have dementia-related symptoms and signs. There is a similar pattern of dementia subtypes across the world, with Alzheimer’s disease and vascular dementia, the two most common forms of dementia, accounting for 50% to 70% and 15% to 25%, respectively, of all dementia cases (Qiu et al. 2009).
Age-related cognitive decline is a main predictor of disability among elderly people, and with the continued expansion of the aging population and the increase in life expectancy, the prevalence of mild cognitive impairment and dementia represented by Alzheimer’s disease have increased (Ogawa S. 2014). Alzheimer’s disease or dementia is prevalent in both nursing facilities and in assisted living/residential care communities, where it affects 45% of older adults (Posthauer et al. 2014).
It has long been known that cognitive function can be influenced by nutrition. There are a variety of nutritional factors, including nutritional status, and dietary patterns, that might be associated with cognitive function, and specific micronutrients and dietary components have been suggested to have an association with cognitive function as well (Ogawa S. 2014). In the elderly, malnutrition and weight loss are indicators of faster progression in Alzheimer’s disease. Patients with early-stage Alzheimer’s disease are more likely to be deficient in specific nutrients, and a low intake of ω-3 fatty acids is associated with an increased risk of mild cognitive impairment and Alzheimer’s disease (Engelborghs et al. 2014).
However, other factors influencing the ability of eating also play an important role in the development of malnutrition in elderlies with cognitive impairment. A study of 155 patients with Alzheimer’s disease showed that swallowing function of severe Alzheimer’s disease patients is poor, and that Alzheimer’s disease is associated with dysphagia (Sato et al. 2014). One in 7 community-dwelling elderlies (14%) with newly diagnosed Alzheimer’s disease is at risk of malnutrition. In a study of 312 community-dwelling Alzheimer’s disease patients, patients at risk of malnutrition were more impaired in basic and complex daily functioning than well-nourished Alzheimer’s disease patients (Droogsma et al. 2013). A study looking at the prevalence of malnutrition in 623 hospitalized elderly patients concluded that elderly patients with dementia had a higher frequency of malnutrition than patients with normal cognition (p<0.0001; odds ratio [OR]=3.2, 95% CI=1.6–6.2). This study also found that the frequency of malnutrition in patients with mild cognitive impairment was significantly higher than in patients with normal cognition (p<0.0001; OR=4.7, 95% CI=2.5–9.0), and was not significantly different from that in patients with dementia (p=0.087; OR 1.1, 95% CI=0.5–2.4) (Orsitto et al 2009).
Osteoarthritis
Osteoarthritis is the most common joint disorder in the United States. Among adults 60 years of age or older, the prevalence of symptomatic knee osteoarthritis is approximately 10% in men and 13% in women. Osteoarthritis has a multifactorial etiology and can be considered the product of an interplay between systemic and local factors (Zhang & Jordan. 2010).
The number of people affected with symptomatic knee osteoarthritis is likely to increase partly due to the aging of the population (Zhang & Jordan. 2010). Pain from osteoarthritis is a key symptom in the decision to seek medical care and is an important antecedent to disability. Because of its high prevalence and the frequent disability that accompanies the disease in major joints such as the knee and hip, osteoarthritis accounts for more difficulty with climbing stairs and walking than any other disease. Osteoarthritis is also the most common reason for total hip and total knee replacement. The rapid increase in the prevalence of this already common disease suggests that osteoarthritis will have a growing impact on health care and public health systems (Zhang & Jordan. 2010).
Age-related macular degeneration
Age-related macular degeneration (AMD) is a disease associated with aging. AMD gradually destroys sharp central vision that is needed for seeing objects sharply and for common daily tasks such as reading and driving. Depending on the stage at diagnosis, AMD may be present as dry AMD, geographic atrophy (advanced form of dry AMD), and wet AMD (choroidal neovascularization). In countries of the Western world, AMD is the leading cause of vision loss in people over the age of 50. It affects about 25-30 million individuals (Richman EA. 2008). AMD has a major influence on quality of life, and as the population ages, more and more people will be affected (Rudnicka et al. 2015).
AMD’s economic impact is profound. According to a report from 2007, the direct medical cost of AMD in the US is approximately 80 million USD / year – not including the cost of lost productivity, the cost of unpaid care from family and friends, nursing home care, or the cost of government programs (Richman EA. 2008).
Diabetes
The prevalence of diabetes mellitus, in general, is growing worldwide, and is becoming an epidemic and endemic problem with the social and economic burden. However, its prevalence and its co-morbidities and mortality are higher in elderlies than in young people. Diagnosed and/or undiagnosed diabetes affects 10.9 million US adults aged 65 years and older, and this number is projected to reach 26.7 million by 2050, which equals to 55% of all diabetes cases. Moreover, 80% of old people have some forms of dysglycemia according to different tests. Thus, diabetes with its complications is one of the most alarming health problems of the current century in middle-aged people and in the elderly (Chentli et al. 2015).
According to the World Health Organization (WHO), the prevalence of diabetes for all age-groups worldwide is estimated to be 2.8% in 2000 and 4.4% in 2030. The total number of people with diabetes is projected to rise from 171 million in 2000 to 366 million in 2030. The most important demographic change to diabetes prevalence across the world appears to be the increase in the proportion of people >65 years of age (Wild et al. 2004).
Osteoporosis
While they may not get as much attention as heart disease, cancer, and other major diseases, bone diseases are common, especially among the elderly, and they take a large toll on the population’s overall health status. Osteoporosis is a disease that leads to an increased risk of fracture due to weakened bone strength. Despite no particular symptoms, the occurrence of fractures leads to death in severe cases. In the case of a femur fracture, 20-30% of patients die within 1 year after the onset of the fracture. The most common cause of osteoporosis is aging, which rapidly progresses after 50 years of age (Looker et al. 2012). Skeletal aging is known to progress faster in women than in men due to hormonal changes after menopause. One out of 6 men (16.7%) and one out of 2 women (50%) have a possibility of experiencing an osteoporosis-related fracture during their lifespan over the age of 50 years (Lee et al. 2013).
The incidence of osteoporosis seems to be higher in patients with Alzheimer’s disease than in patients in the same age group without memory impairment, and the treatment as well as rehabilitation are more difficult in the former group. Less than half of these patients can regain their previous functional status after a fracture (Tysiewicz-Dudek et al. 2008).
NUTRITIONAL NEEDS IN ELDERLIES
Change in nutritional needs may be related to the normal aging process, medical conditions, or lifestyle in elderlies (Amarya et al. 2015). Old people tend to have dehydration, protein-energy malnutrition, and an inadequate intake of energy, protein, fat-soluble vitamins, minerals, and trace elements, partly due to a more carbohydrate-rich diet (Amarya et al. 2015).
Nutritional needs change throughout life. Especially for the elderly, these changes may be related to the normal aging process, medical conditions, or lifestyle (Amarya et al. 2015).
Age-related changes relevant to nutrition (Amarya et al. 2015).
Energy
Elderly people require less energy than young adults because of a reduced basal metabolic rate; as a result, there is a reduction in the levels of activity. Energy requirement is dependent on a number of factors, including age, gender, body composition, weight, and activity levels. Generally, energy requirements decrease due to loss of fat-free mass. As a consequence, resting energy expenditure is found to be lower in elderly individuals than in young adults. In those older people who have very low energy requirements, there is a risk of their diet not meeting micronutrient requirements; the quality of diet is therefore of prime importance to ensure that deficiencies do not develop. Older people should be encouraged to meet their energy requirement through a healthy diet (Amarya et al. 2015).
Protein
Protein is necessary for building up muscles, and to replenish vital body fluids and wear and tear of the body. It is also required for the metabolic processes of the body in the form of enzymes and hormones. Older persons are vulnerable to protein–energy malnutrition associated with a progressive decline in body protein manifested by declining fat-free mass. The reduction in fat-free mass is attributed mainly to the loss of skeletal muscle and is associated with reduced muscle strength as well as predisposition to many metabolic disorders. The requirement of protein for older persons is 0.91–1 g/kg/day. Adequate protein intake can be achieved by the inclusion of milk and milk products, eggs, meat, fish, and chicken, as well as legumes and nuts in the diet (Amarya et al. 2015).
Fat
Fat is a concentrated source of energy. It makes food palatable and helps in the absorption of fat-soluble vitamins such as vitamins A, D, E, and K. It is desirable to include a variety of fats in the diet, particularly ω-3 fatty acids found in fish, soy, linseed, canola seed and oil, seaweed, and green leaves (Amarya et al. 2015).
Carbohydrates
During old age, loss of teeth makes it difficult to chew food properly. Elderly people tend to consume more carbohydrate-rich food that require minimum chewing, are easily digested, need minimum cooking time, stand maximum storage, and are cheaper than protein-rich food. Care should be taken to restrict the amount of sugar and refined cereals in the diets, and to include whole cereals, fiber-rich fruits, and vegetables instead (Amarya et al. 2015).
Vitamins, minerals, and trace elements
Calcium and vitamin D help maintain good bone health. Therefore, it is advisable to increase the intake of calcium-rich food such as milk, and milk products such as cottage cheese and curd, green leafy vegetables, and sesame seeds. If elderly people are confined indoors and are not exposed to sunshine, they should be given vitamin D supplements (Amarya et al. 2015).
Anemia is another common nutritional problem in old age, and efforts must be made to include iron-rich green leafy vegetables, fresh food, rice flakes, etc. in the diets of elderly people (Amarya et al. 2015).
Vitamin A (β-carotene), vitamin E, and vitamin C are protective antioxidants. Liberal intake of food rich in β–carotene, such as green, yellow, and orange vegetables and fruits, is advocated due to their antioxidant properties. Citrus fruits, green leafy vegetables, cabbage, green chilies, guava, and sprouted vegetables are rich sources of vitamin C. Folate, found in green leafy vegetables, pork, liver, sprouts, groundnuts, and oilseeds, is associated with a diminished risk of vascular disease. In addition to the recognized essential nutrients, there are many other food components, collectively known as phytochemicals, that can lower the risk of major health problems such as cancer and heart disease. Hence, consumption of food rich in phytochemicals, such as green tea, red wine, garlic, tomatoes, and so on should be encouraged. Vitamin deficiencies, particularly vitamins B12, B6, and folate, are associated with cognitive impairment (Amarya et al. 2015).
Nutritional interventions have an impact on vascular disease prevention. Emerging research suggests that supplementation with ω-3 fatty acids (the precursors of anti-inflammatory mediators) and consumption of cruciferous vegetables are all associated with stroke prevention and may be beneficial if integrated into the diet of all elderly patients with vascular disease or vascular risk factors. Other important antioxidants with possibly beneficial outcomes include food with high levels of phytochemicals and flavonoids. Tomatoes, citrus fruit, blueberries, and certain spices are known to reduce oxidative stress and cognitive impairment (Amarya et al. 2015).
Fluids
Many degenerative age-related diseases aggravate the tendency toward dehydration in older persons. Generally, adults require about 30 ml/kg of fluids per day. These fluids need not be restricted to water only and may include other fluids such as milk, juices, soft drink, soup, tea, and coffee. However, tea and coffee should be taken in moderate amounts only (Amarya et al. 2015).
MALNUTRITION IN ELDERLIES
Nutrition is an important determinant of health in elderly patients. Chronic conditions often seen in these patients may lead to disease-related malnutrition (Allepaerts et al. 2014, Amarya et al. 2015). Malnutrition is associated with numerous poor health outcomes, including high mortality rates, poor physical functioning, and increased healthcare costs in older adults (Suominen et al. 2014, Pirlich et al. 2006, van der Pols-Vijlbrief et al. 2014, van Stijn et al. 2013).
Disease-related malnutrition
Disease-related malnutrition is the type of malnutrition that is triggered by illness or disease. It is the primary reason for malnutrition in developed countries, especially in the elderly, since many of the diseases triggering malnutrition are related to age. The most common diseases that can cause malnutrition include oncological diseases such as cancer, pulmonary diseases such as chronic obstructive pulmonary disease or cystic fibrosis and gastroenterological diseases such as inflammatory bowel disease. Certain treatments of these diseases can also have a negative impact on nutrition, like chemotherapy or radiation therapy.
Malnutrition is as much a cause as a consequence of ill health: a poor food intake, especially for a prolonged period, makes us more prone to illness and injury that can lead to a reduced appetite through a wide variety of mechanisms – which results in poor food intake. It is a vicious cycle which often requires medical help to stop.
Factors contributing to the development of malnutrition
Malnutrition in the elderlies
Over the past decades, the importance of nutritional status in the elderly has increasingly been recognized in a variety of morbid conditions such as cancer, heart disease, and dementia. Nutrition is an important determinant of health in elderly patients. Nutritional status assessment is essential for preventing or maintaining various chronic and acute diseases, and even for healing. As people age, various changes occur in the body, which may or may not affect the nutritional status of an individual. A common problem related to aging is loss of bone density, which can increase the risk for osteoporosis. Sarcopenia is the other age-related change. The loss of lean body mass can lead to a gain in body fat. Muscle loss is seen even in healthy people, which implies that metabolic changes occur during aging, making it a universal phenomenon. It may be more noticeable by loss of strength, functional decline, and poor endurance. This loss also leads to reduced total body water content. Various other changes occur throughout the digestive system. There is a decrease in gastric acid secretion, which can limit the absorption of iron and vitamin B12. Saliva production decreases, leading to slower peristalsis and constipation. Appetite and thirst dysregulation also occurs. Sensory changes affect the appetite in many ways. Vision loss makes cooking, and even eating, more difficult. Diminished senses of taste and smell make the food less appealing. These changes typically alter eating habits and reduce nutrient availability and absorption, which can lead to nutritional deficiencies and various health problems (Amarya et al. 2015).
Aging causes alterations in the body composition, organ functions, adequate energy intake, and ability to eat or access food. Aging of the body predisposes to a high incidence of undernutrition in the elderly persons wherever they are living, but the prevalence of malnutrition is particularly high in hospitalized or institutionalized patients. Numerous conditions in relationship with physiological aging, comorbidity, polymedication, and the way of life of the individuals predispose them to malnutrition (Allepaerts et al. 2014, Amarya et al. 2015). Aging is associated with an increased risk of malnutrition, decreased nutrient intake, unintentional weight loss and sarcopenia, which lead to frailty, functional disabilities, and increased mortality (Suominen et al. 2014). Chronic diseases – diseases that interfere with the ability of eating food, such as stroke, dental problems, malabsorption syndromes, cardiac cachexia, chronic obstructive pulmonary disease, malignant diseases, neurologic disorders, dementia -, psychological disturbances, and social problems can also result in decreased food intake (Saka et al. 2010). All these conditions may result in the development of malnutrition (Amarya et al. 2015).
Factors that contribute to malnutrition in the elderly (Amarya et al. 2015).
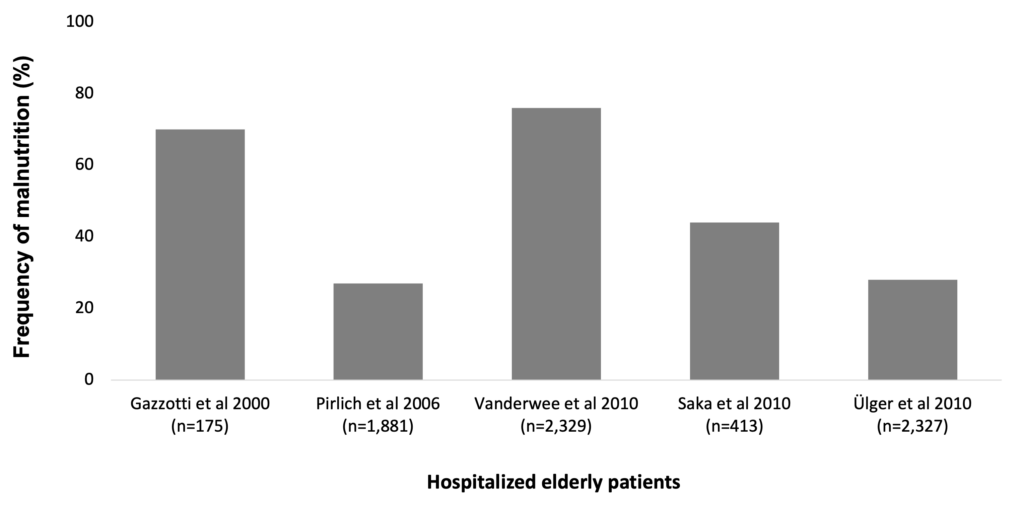
Malnutrition is a serious and frequent condition in older adults. Several studies have found different rates of malnutrition and being at risk of malnutrition in the elderly. In a large Belgian regional hospital study, of the 175 elderly patients (mean age 79.7±8.5 years) enrolled, 48.6% were at risk of malnutrition and 21.7% were found to be severely malnourished (Gazzotti et al. 2000). In a study of 2,329 elderly patients (aged 75 years or older) across elderly wards in Belgium, 33% was found to suffer from malnutrition and 43% was at risk of malnutrition (Vanderwee et al. 2010). According to two Turkish studies on malnutrition among the elderly, frequency of poor nutritional status is between 28% (Ülger et al. 2010) and 44% (Saka et al. 2010).
Frequency of malnutrition is 30-60% among hospitalized or institutionalized elderly patients (Gazzotti et al. 2000, Pirlich et al. 2006, Vanderwee et al. 2010, Saka et al. 2010, Ülger et al. 2010)
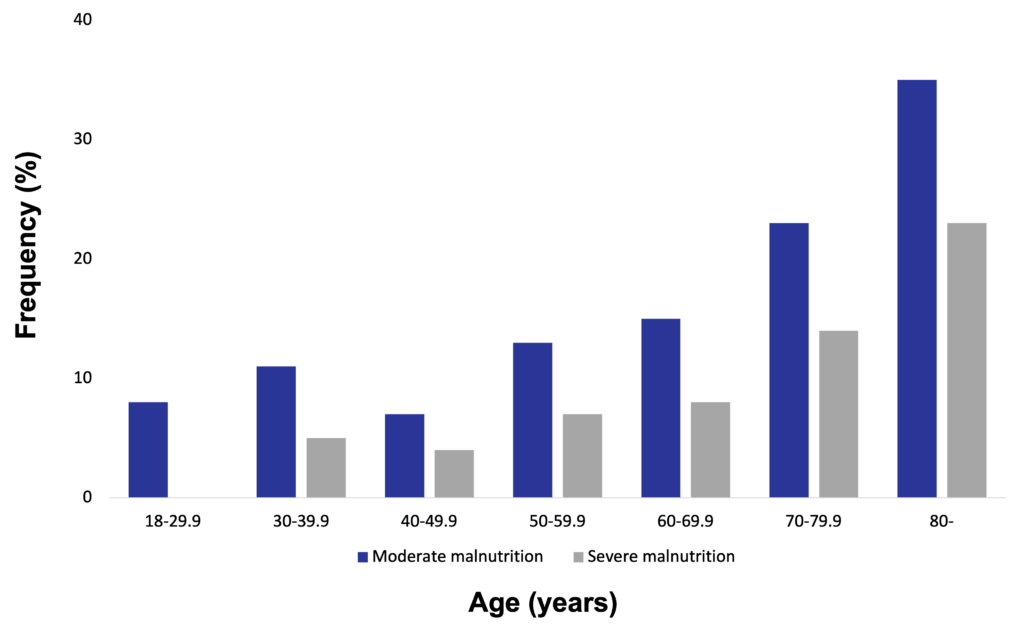
A German hospital malnutrition study conducted in 1,886 consecutively admitted patients in 13 hospitals found that 27.4% of these patients were malnourished. Based on subjective global assessment, 17.6% were classified as moderately malnourished, and 9.8% as severely malnourished. Of patients aged ≥70 years, 43% were malnourished, with 16.7% classified as severely malnourished. In comparison, only 7.8% of patients aged <30 years were malnourished, and none were classified as severely malnourished. The highest prevalence of malnutrition was found in geriatric departments, followed by oncology and gastroenterology departments (Pirlich et al. 2006).
Among hospitalized patients, malnutrition is more frequent in the elderlies (Pirlich et al. 2006)
In general, the prevalence of malnutrition is about 5-10% among independently living older individuals but is considerably higher (30-60%) in hospitalized or institutionalized older adults (Ülger et al. 2010).
There are many psychological, social, and organic conditions related to malnutrition in the elderly (Ülger et al. 2010). Certain conditions are associated with a significantly higher prevalence of malnutrition in older patients. These conditions include old age, coming from a nursing home, having COPD, cancer, pneumonia, urinary infection, decompensated heart failure, delirium, dementia, depression, taste difficulties, swallowing difficulty, digestion problems, pain, mouth infection, chewing difficulty and a longer hospital stay (Vanderwee et al. 2010).
Consequences of malnutrition in the elderlies
Sarcopenia, an aging-induced generalized decrease in muscle mass, strength, and function, is known to affect elderly individuals by decreasing mobile function and increasing frailty and imbalance that lead to falls and fragility fractures. Sarcopenia has been reported to affect more than 40% of elderly individuals older than 70 years of age, approximately 50 million people worldwide. This number is estimated to increase to 500 million by the year 2050. Sarcopenia is believed to be caused by multiple factors such as disuse, malnutrition, age-related cellular changes, apoptosis, and genetic predisposition. The etiology of sarcopenia comprises a wide variety of causes that are involved in a complex manner, including disuse secondary to comorbidities (malnutrition, vitamin D deficiency, cerebral infarction, heart failure, and osteoarthritis) as well as age–related hormonal changes (involving testosterone, estrogen, insulin-like growth factor 1, and insulin), apoptosis, denervation, and changes in inflammation and immunity involving interleukin (IL)-1, IL-6, and tumor necrosis factor (TNF)-α, social causes, and mental causes such as decline in cognitive function or decrease in social activity. It has been reported that in the histological examination of muscle fibers, type II muscle fibers (in other words, the so-called fast muscles) decrease with age, while type I muscle fibers (in other words, the so-called slow muscles) are preserved (Hida et al. 2013).
Protein-energy malnutrition is associated with numerous poor health outcomes, including high health care costs, mortality rates, and poor physical functioning in older adults. Risk factors of protein–energy malnutrition are poor appetite, edentulousness, having no diabetes, hospitalization, and poor self-reported health (van der Pols-Vijlbrief et al. 2014). A German hospital malnutrition study conducted in 1,886 consecutively admitted patients in 13 hospitals found that malnutrition was associated with a 43% increase of hospital stay (p<0.001) (Pirlich et al. 2006).
A systematic literature review of 10 consecutive years (1998-2008) showed that serum albumin and ≥10% weight loss in the previous 6 months are significant preoperative predictors of postoperative outcome in elderly general surgery patients (van Stijn et al. 2013).
NUTRITIONAL THERAPY IN ELDERLIES
Most elderly subjects have insufficient calorie and protein intake (Shock MW. 2015). Low-volume, nutrient- and energy-dense oral nutritional supplements improve nutritional status (Stange et al. 2013), while high protein intake improves muscle mass and strength (Hayashi et al. 2020, Hida et al. 2013).
Nutritional deficiencies in elderlies can be avoided as long as the diet is varied to assure adequate intake of all nutritional elements. Deficiencies are most likely to develop from poor eating habits, such as excessive intake of carbohydrate with a reduction in protein. In the elderly, these deficiencies are most apt to be in the intake of protein, calcium, iron, vitamin A, and thiamine (Shock MW. 2015).
Most elderly subjects have insufficient calorie and protein intake, and the combination of exercise and dietary supplements containing amino acids and proteins may have an effect on sarcopenia and result in a short-term increase in muscle mass and muscle strength, even in the elderly. Due to the multifactorial etiology of sarcopenia in elderlies, the development of a specific treatment is quite difficult, and evidence of effective treatment is limited. One of the therapeutic methods that are currently being attempted is nutritional therapy.
A randomized controlled interventional trial of elderly nursing home residents with high functional impairment showed that a low-volume, nutrient- and energy-dense oral nutritional supplement (ONS) administered for 12 weeks was well accepted and resulted in significant improvement of nutritional status and, thus, was effective to support the dietary management of malnutrition (Stange et al. 2013).
A low-volume, nutrient- and energy-dense oral nutritional supplement resulted in significant improvements of nutritional status in elderly nursing home residents (Stange et al. 2013)
In a 9-month randomized controlled trial examining the combination of dietary supplements and exercise showed that in 42 out of the 57 elderly women examined, dietary intervention based on nutritional supplement drinks containing proteins, and exercise therapy resulted in improved muscle strength (Hida et al. 2013).
In a study of 157 pre-frail or frail elderly individuals, total and per meal protein intake (by food questionnaires), total and appendicular lean mass (by DEXA), vastus lateralis cross-sectional area (by B-mode ultrasound), and muscle function (by leg-press and bench-press, timed-stands test and go test, handgrip, and risk of falls) were determined. Protein intake and number of meals with either ≥20 g or ≥30 g of protein were significantly associated (after controlling for confounding factors) with greater total and appendicular lean mass and vastus lateralis cross-sectional area (Hayashi et al. 2020).
It is crucial to use ONS with the most appropriate composition to ensure optimal nutritional therapy for elderlies with different chronic conditions. ONS use, taurine and increased ω-3 fatty acids intake beneficially affect the risk of developing dementia and Alzheimer’s disease (Lauque et al. 2004, Zhang et al. 2020, Chupel et al. 2018, Morris et al. 2003, Barberger-Gateau et al. 2002).
Nutritional therapy in elderly patients with cognitive impairment / Alzheimer’s disease
Findings from 26 patients over the age of 65 with dementia indicate that supplement drinks may be beneficial in reducing the prevalence of malnutrition within the group as more people meet their nutritional requirements. As the provision of supplement drinks is also demonstrated to have an additive effect to consumption of habitual foods, these can be used alongside other measures to also improve oral intake. Moreover, in a meta-analysis, ONS had a positive effect on cognitive functions as well (Allen et al. 2013).
In a study of 91 subjects with Alzheimer’s disease aged ≥65 years and at risk of undernutrition evaluated by the Mini Nutritional Assessment (MNA score ≤23.5), oral nutritional supplementation for 3 months significantly improved energy and protein intakes in the intervention group (n=46), resulting in a significant increase in weight and fat-free mass. At 3 months, weight gain occurred more often in the intervention group (71.4% vs 41.8%), while weight loss (≤4% of body weight), and significant weight loss (>4% of body weight) occurred less often in the intervention group (17.1% vs 32.6% and 11% vs 26%, respectively). The nutritional benefit was maintained in the intervention group after discontinuation of oral supplementation at 3 months. Oral supplementation was also proven to be practicable and effective, and the patients accepted it well. The improvement that was observed even in the control group (n=45) showed that caregiver education is an important factor in maintaining the nutritional status of patients with Alzheimer’s disease. Moreover, regular courses of oral supplementation may help maintain the increase in fat-free mass and improve the nutritional status of these patients (Lauque et al. 2004).
ONS improves weight in Alzheimer’s disease patients who are at risk of malnutrition (Lauque et al. 2004)
Taurine, 2-aminoethanesulfonic acid, is the second most abundant endogenous amino acid in the central nervous system (CNS) and plays multiple roles in the human body: thermoregulation, stabilization of protein folding, anti-inflammatory effects, antioxidation, osmoregulation, calcium homeostasis and CNS development. Due to its nontoxic and curative properties, taurine is frequently found in food, drinks, and drugs for treating liver and heart disorders. Recently, taurine has shown therapeutic effects as a cognitive enhancer in animal models of non-Alzheimer’s disease neurological disorders. Taurine recovers memory impairments induced by alcohol, pentobarbital, sodium nitrite, and cycloheximide in mice without any observable effects on other behaviors including motor coordination, exploratory activity, and locomotor activity. Cognitive deficits of rats from excess manganese exposure are improved, and upregulated acetylcholinesterase activity is partially restored after taurine administration. The intracerebroventricular administration of taurine protects mice from hypoxia-induced learning impairment. In addition, intravenously administered taurine significantly improves post-injury functional impairments of traumatic brain injury in rats. Taurine supplementation has also been found to rescue aging-dependent loss of visual discrimination in mice. In streptozotocin-induced sporadic dementia rat models, cognitive impairment and abnormal acetylcholinesterase activity is ameliorated by taurine (Kim et al. 2014).
Taurine also has multiple disease-modifying roles to prevent or cease neuropathology of Alzheimer’s disease. Anti-inflammatory and antioxidant properties of taurine also protect neuronal cells and mitochondria from neurotoxicity of amyloid-β (Aβ). By activating gamma amino-butyric acid (GABA) and glycine receptors, taurine inhibits excitotoxicity caused by Aβ-induced glutamatergic transmission activation. Taurine is also observed to attenuate Aβ-associated neuronal cell death, mitochondrial permeability transition pore opening, mitochondrial dysfunction, and intracellular reactive oxygen species generation (Kim et al. 2014). In a water maze reference memory study, mice given taurine supplementation (100 and 400 mg/kg body weight/day) besides D-galactose treatment (100 mg/kg body weight/day) spent shorter (p<0.05) time in searching target than mice in the control group. Moreover, taurine supplementation significantly extended (p<0.05) the searching period around the target quadrant in the probe test of the water maze, and neuronal degeneration and nucleus shrinkage in the hippocampus dentate gyrus area of D-galactose treated mice were observed to be attenuated. Taurine also downregulated (p<0.05) the expression of the glial fibrillary acidic protein and of the cluster of differentiation marker Cd11b; meanwhile, it strengthened (p<0.05) the antioxidant capacity and lowered (p<0.05) the accumulation of advanced glycation end-products in the brain (Tu et al. 2018). In another animal study, taurine supplementation at 250 mg/kg/day improved cognitive deficits in oligomeric Aβ-infusion-treated mice to a similar extent as the previously determined concentration of 1000 mg/kg/day (Kim et al. 2014). In addition, in an AD mouse model study, it was found that taurine directly binds to oligomeric Aβ. Given that oligomeric Aβ induce cognitive impairment by binding to selective receptors in neuronal synapses, enhancement of learning and memory in the oligomeric Aβ-infusion mouse model suggests that taurine may prevent memory deficits by direct binding to oligomeric Aβ (Jang et al. 2017).
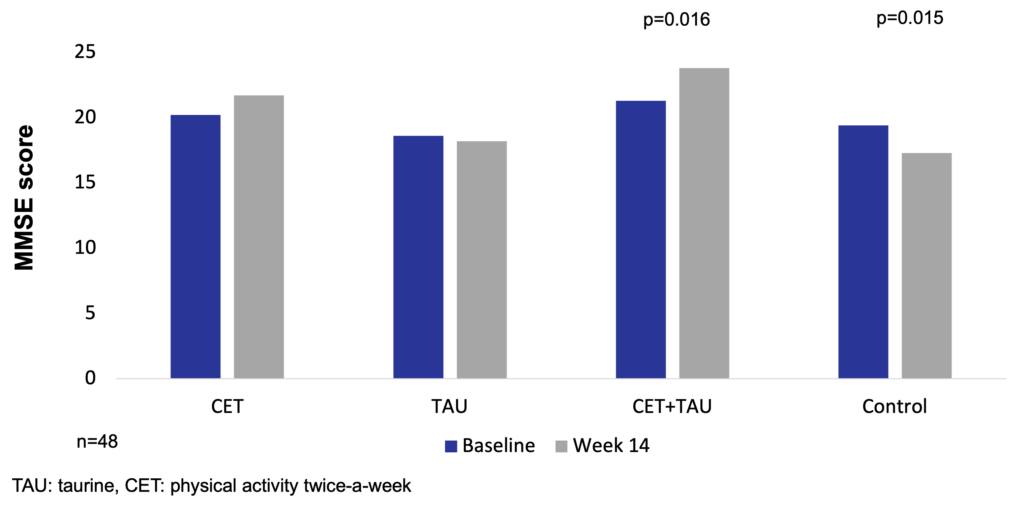
In a naturalistic, prospective, 14-week controlled trial of 48 elderly women, the Mini Mental State Examination (MMSE) score increased in the group receiving 1.5 g/day taurine supplementation combined with exercise treatment twice a week (CET+TAU, n=11) (p<0.05) versus the 1.5 g/day taurine supplementation only group (TAU, n=12), the combined exercise training twice a week only group (CET, n=13), and the control group (CG, n=12). Concentrations of the neuronal-derived protein S100β were maintained in all intervention groups, while a subtle increase in the control group was found. Neurospecific enolase levels increased only in the taurine supplemented group (p<0.05). Combined exercise treatment reduced TNFα, IL-6, and IL-1β/IL-1ra, IL-6/IL10, and TNFα/IL-10 ratios (p<0.05). Taurine supplementation decreased the IL-1β/IL-1ra ratio (p<0.05). Multiple regression analysis showed that there was a trend for changes in IL-1β and the Charlson Comorbidity Index to be independently associated with changes in S100β. Exercise and taurine decreased inflammation and maintained the blood-brain barrier integrity in elderly women (Chupel et al. 2018).
Taurine supplementation with combined exercise treatment increases MMSE score in elderly women (Chupel et al. 2018).
A significant component of membrane phospholipids in the brain is the ω-3 long-chain polyunsaturated fatty acid (PUFA) docosahexanoic acid (DHA). High levels of DHA are found in the metabolically more active parts of the brain, such as the ceberal cortex, the mitochondria, the synaptosomes, and the synaptic vesicles. DHA intake in humans is provided either by fish oil in the diet or is synthetised from its precursors (𝛼-linolenic acid / ALA, and eicosapentaenoic acid / EPA) present in food (Morris et al. 2003). In animal studies, ω-3 PUFA supplementation resulted in better laboratory parameters, and superior learning acquisition and memory performace compared to control animals (Morris et al. 2003).
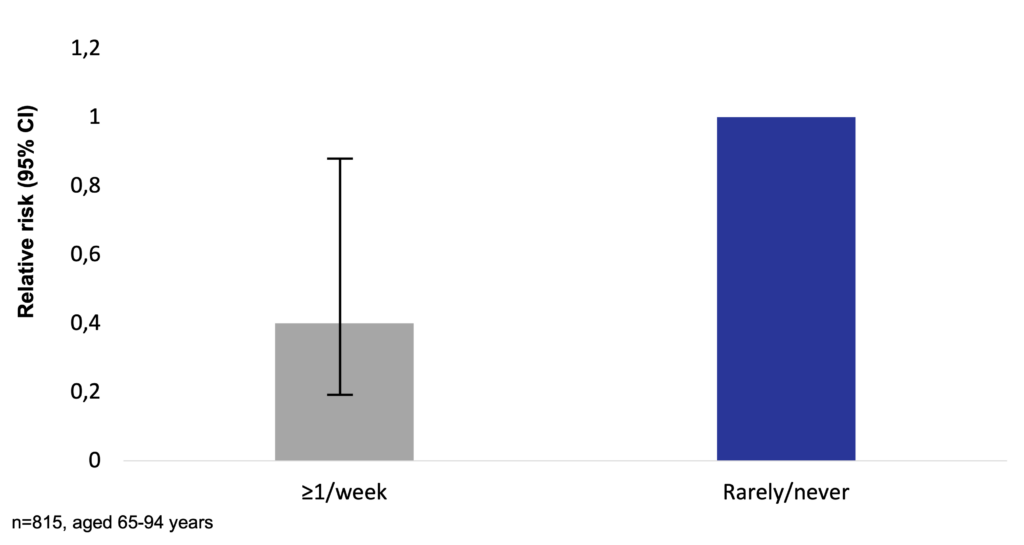
In a prospective study of 815 residents aged 65-94 years and initially not affected by Alzheimer’s disease, fish consumption of at least once a week was associated with a 60% less risk for developing Alzheimer’s disease compared to fish consumption of rarely or never (RR=0.4, 95% CI: 0.2-0.9). Total intake of ω-3 PUFA was associated with a decreased risk of developing Alzheimer’s disease (Morris et al. 2003).
Fish consumption and ω-3 fatty acids intake decreases the risk for developing Alzheimer’s disease (Morris et al. 2003)
In a study of 1,674 elderly French participants aged ≥68 years and living at home, frequency of consumption of meat and fish or seafood has been recorded as daily, at least once a week (but not every day), from time to time (but not every week), and never. During 7 years of follow-up, 170 new cases of dementia occurred, of which 135 cases were Alzheimer’s disease. A significant trend has been found between increased fish and seafood consumption and decreased incidence of dementia (ptrend=0.0091). There was no significant association between meat consumption and risk of dementia (ptrend=0.59) (Barberger-Gateau et al. 2002).
ω-3 fatty acids intake affects the development of dementia and Alzheimer’s disease (Barberger-Gateau et al. 2002)
In a meta-analysis of 7 studies with a total of 213 cases of intervention and 221 cases of placebo, compared with placebo, ω-3 PUFA supplements effectively improved cognition in elders with mild cognitive impairment (weighted mean difference: 0.85, 95% CI: 0.04–1.67, p=0.04) (Zhang et al. 2020).
Lutein and zeaxanthin may ameliorate age-related macular degeneration (Garcia-Layana et al. 2013, Huang et al. 2015, Dawczynski et al. 2013), and Salto3TM may improve joints condition (Salto3TM Quality Statements 2006).
Nutritional therapy in elderly patients with age-related macular degeneration
Macular pigment is comprised of the carotenoids lutein, zeaxanthin, and meso-zeaxanthin, which selectively accumulate at the macula (central retina) of the eye and are neuroprotective. These carotenoids are also present in the brain, and evidence suggests a close correlation between retinal and brain concentrations (Feeney et al. 2013). Within the central macula, up to 75% of the pigments is zeaxanthin, whereas in the peripheral retina lutein predominates (≥67%). Lutein and zeaxanthin are thought to reduce oxidative damage by filtering short-wavelength blue light within the macula and by quenching light-induced singlet oxygen and related free radicals. Oxidative stress is thought to increase the risk of AMD development – thus, the role of antioxidant treatment is of interest (Berrow et al. 2013).
In a study of 4,453 adults aged ≥ 50 years investigating the relationship between macular pigments and cognitive function, lower macular pigment optical density (MPOD) was associated with poorer performance on the MMSE (p=0.026) and on the Montreal cognitive assessment (p=0.016). Individuals with lower MPOD also had poorer prospective memory (p=0.011), took longer time to complete a trail-making task (p=0.003), and had slower and more variable reaction times on a choice reaction time task (p=0.000 and p=0.001, respectively) (Feeney et al. 2013).
Low carotenoid status (especially of the xanthophylls lutein and zeaxanthin) is common in older adults and has been associated with a number of degenerative diseases of the central nervous system ranging from retina (e.g., macular degeneration) to brain (e.g., Alzheimer’s disease). A study of 24 subjects with mild cognitive impairment found that when compared to age-, body mass index (BMI)-, ethnicity-, sex-, and smoking-status-matched controls (n=24), MPOD was broadly related to cognition including the composite score on the MMSE (p=0.02), visual-spatial and constructional abilities (p=0.04), language ability (p=0.05), attention (p=0.03), and the total scale on the Repeatable Battery for the Assessment of Neuropsychological Status (p=0.03) (Renzi et al. 2014). Based on the above findings, several studies have investigated whether xanthophyll supplementation influences MPOD and thus the vision in older patients. A small prospective study of 44 patients with early AMD demonstrated that compared to the placebo group, 1-year daily nutritional supplement of 12 mg of lutein, 0.6 mg of zeaxanthin, and 280 mg of DHA significantly increased the mean MPOD (0.059 vs 0.162, p<0.05) (Garcia-Layana et al. 2013). In a study of 112 patients with early AMD randomly (1:1:1:1) assigned to receive 10 mg lutein, 20 mg lutein, 10 mg lutein+10 mg zeaxanthin, or placebo daily for 2 years, supplementation with lutein and zeaxanthin augmented MPOD significantly in active treatment groups (all p<0.05) (Huang et al. 2015).
Supplementation with lutein and/or zeaxanthin increases MPOD in patients with early age AMD (Huang et al. 2015)
The double-blind, placebo controlled LUTEGA study of 172 patients with non-exudative AMD investigated the effects of supplementation with either once (D1) or twice (D2) daily of 10 mg lutein + 1 mg zeaxanthin + ω-3 long-chain polyunsaturated fatty acids (thereof 100 mg DHA, 30 mg EPA) + antioxidants, or placebo. After 12 months of intervention, the MPOD parameters (volume, area, maximal optical density, mean optical density) increased significantly in treatment arms D1 and D2 (p<0.001). Volume of MPOD showed the highest within-group difference and increased significantly in D1 and D2 and decreased significantly in the placebo group (p=0.041). Between-group comparison of absolute changes of all MPOD parameters were significantly different between D1 and placebo as well as D2 and placebo with p<0.001 at end point. Best-corrected visual acuity (BCVA) improved in D1 and in D2 (p<0.001). After 12 months of intervention, the mean improvement in BCVA was significant both in D2 (p=0.006) and D1 (p=0.038) compared to placebo (Dawczynski et al. 2013).
Nutritional therapy in elderly patients with osteoarthritis
Inflammation is a consequence of joint disorders, but it can also be considered as a cause, because inflammation maintains and encourages degeneration. In in vivo studies conducted on mice, compared to anti-inflammatory agents ibuprofen and aspirin, Salto3TM reduced inflammation, both cause and consequence of joint pain (Salto3TM Quality Statements 2006).
In a single-center, randomized, placebo-controlled, double blind, 90-day clinical study designed to assess the efficiency of Salto3TM to reduce joint pain in 60 years old subjects (n=57) suffering from mild to moderate osteoarthrosis of the knee, Salto3TM helped reduce the feeling of pain in the subgroup of volunteers with a nascent osteoarthrosis (n=12) by almost 50% (p=0.0094) (Salto3TM Quality Statements 2006).
COMPLIANCE TO ORAL NUTRITIONAL SUPPLEMENTS IN ELDERLIES
Compliance significantly influences cost-effectiveness. With the proper characteristics, such as high energy-density, being milk-protein based, and availability in preferred flavors, ONS lead to good compliance, and thus improve the nutritional status of elderlies (Stange et al. 2013, Hubbard et al. 2012, Darmon et al. 2008).
Energy content
Just like for any other therapeutic approach, one of the major questions of nutritional supplementation is compliance that significantly influences cost-effectiveness. Although ONS are known to be effective to treat malnutrition in the elderly, a known barrier for ONS use among elderlies is the volume that needs to be consumed, with a high-volume need resulting in low compliance and thus reduced effectiveness (Stange et al. 2013). Clinical studies show that overall compliance to ONS is good, 78% (67% in hospital, 81% in community). Compliance is significantly higher with ONS of higher energy-density (≥2 kcal/ml) than with ONS of lower energy content (1.5 kcal/ml and 1-1.3 kcal/ml), while there is no significant difference in compliance between ONS of 1.5 kcal/ml and ONS of 1-1.3 kcal/ml (Hubbard et al. 2012).
Compliance is greater with higher energy-density ONS (Hubbard et al. 2012).
A randomized controlled intervention trial of 77 elderly nursing home residents with high functional impairment showed that a low-volume, nutrient- and energy-dense oral nutritional supplement was well accepted and resulted in significant improvements of nutritional status and, thus, was effective to support treatment of malnutrition (Stange et al. 2013).
Taste
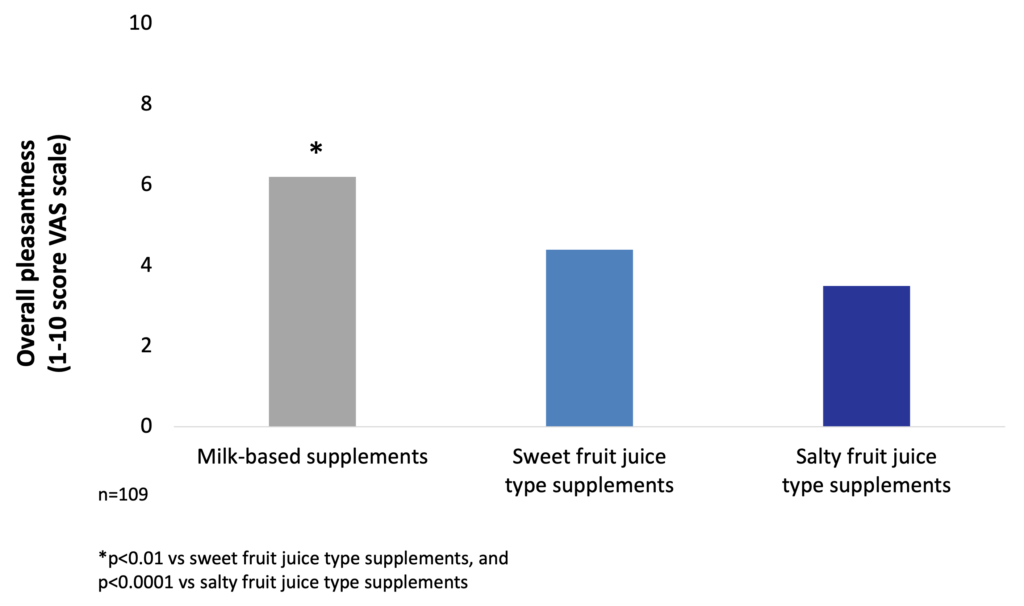
The investigation of taste preferences of milk-based and fruit juice-type ONS in malnourished in-patients showed that milk-based products are significantly more frequently preferred than fruit-juice typed supplements (81.6% vs 18.4%, p<0.001). Moreover, the overall pleasantness is also significantly better for milk-based supplements than for fruit juice-type products (Darmon et al. 2008).
Pleasantness of milk-based ONS is significantly better than that of sweet or salty fruit juice-type products (Darmon et al. 2008).
Compliance is also influenced by patients’ taste-preferences: of the milk-based supplements, coffee, vanilla, and strawberry are the most preferred flavors (Darmon et al. 2008).
Among milk-based products, coffee, strawberry, and vanilla are the most preferred flavors (Darmon et al. 2008).
COST-EFFECTIVENESS of ORAL NUTRITIONAL SUPPLEMENTS IN ELDERLIES
ONS are cost-effective in the nutrition of malnourished elderlies (Neelemaat et al. 2011, Neelemaat et al. 2012, Freijer et al. 2012, Nuijten and Mittendorf. 2012).
Cost-effectiveness of oral nutritional supplements in elderlies
Efficacy and cost-effectiveness of ONS have been investigated in community-dwelling elderly people as well. Regardless of the country or the screening tool used, the prevalence of elderlies at risk for malnutrition is approximately 32-34%. A higher risk of malnutrition has been linked to older age, disability, medical illnesses, previous admission to a hospital, low education level, cognitive impairment, smoking, loss of a spouse, and low baseline body weight (de van der Schueren et al. 2014). Insufficient dietary intake in community-dwelling elderlies has deleterious consequences on physical and cognitive functioning and clinical outcomes. Conversely, several factors associated with aging influence dietary need and prevent consumption of a nutritious diet. Thus, older people are vulnerable to malnutrition that leads to negative clinical outcomes and increased health costs. Neelemat et al. investigated effectiveness of nutritional supplementation (treated group) compared to standard care (control group) in 210 older (>60 years of age) malnourished patients in a randomized controlled trial. Participants received the assigned therapy for 3 months post-discharge. Results showed that ONS in malnourished elderlies increased body weight (mean difference 3.4 kg) and decreased functional limitations compared to standard care (Neelemaat et al. 2011). Cost-effectiveness analysis revealed that the significant improvement in functional limitations was achieved with no extra costs (Neelemaat et al. 2012).
A health economic – budget impact analysis performed in the Netherlands to assess the economic impact of using ONS for the treatment of disease-related malnutrition on the national health care budget demonstrated that using ONS in community-dwelling elderlies leads to a total annual cost savings of € 13 million (18.9% savings), when all eligible patients are treated. The additional costs of ONS (€ 57 million) are more than balanced by a reduction of other health care costs, for example, (re-)hospitalization (€ 70 million) (Freijer et al. 2012).
Using ONS in community dwelling elderlies leads to cost savings (Freijer et al. 2012)
A German study assessing the health economic impact of ONS showed that the extra costs for ONS (€ 534) are off-set by a reduction of hospitalization costs (€ 768) leading to total cost savings of € 234 per patient (Nuijten and Mittendorf. 2012).
Use of ONS leads to cost savings for the cost of disease-related malnutrition in the hospital setting (Nuijten and Mittendorf. 2012)
MEDIDRINK PLATINUM
MediDrink Platinum is a 2.0 kcal/ml, complete, lactose- and gluten-free food for special medical purposes for the the dietary management of disease-related malnutrition primarily in elderlies.
MediDrink Platinum is not suitable for children below 3 years of age, and for patients with galactosemia and hereditary fructose intolerance (fructosemia). The dosage of MediDrink Platinum administered should be decided by a physician.
MediDrink Platinum is available in 4 different flavors: chocolate, coffee, strawberry, and vanilla.
Product description
MediDrink Platinum is a nutritionally complete, 2.0 kcal/ml, food for special medical purposes for the dietary management of disease-related malnutrition primarily in elderlies.
MediDrink Platinum must be used under medical supervision.
MediDrink Platinum is suitable as a sole source of nourishment or as a supplemental nutrition. MediDrink Platinum is for enteral use only.
Product composition
All micronutrient levels in MediDrink Platinum comply with the EC Directive 128/2016 minimum and maximum levels. There are other components in MediDrink Platinum that are already registered and are in use to ameliorate certain conditions often seen in elderly people. Quantities of these components are in accordance with their dosing recommendations.
Download MediDrink Platinum Product Information Sheet
Target groups
MediDrink Platinum is indicated for per os feeding to enhance the energy, protein, and micronutrient intake of elderly patients with disease-related malnutrition. MediDrink Platinum is suitable for all patients with a functional gastrointestinal tract who are unable to meet the nutritional requirements with food intake alone.
MediDrink Platinum is specifically suitable for:
- older patients with or at risk of malnutrition, requiring enteral nutritional supplementation
- older patients with cachexia
MediDrink Platinum is lactose-free (contains lactose ≤0.1 g / 100 g), and is gluten-free, therefore, can be administered to patients with lactose- or gluten-intolerance.
Recommended dosage
The quantity of MediDrink Platinum administered should be decided by the treating physician and varies from patient to patient according to individual needs and whether MediDrink Platinum is used as supplemental nutrition or as the sole source of nutrition.
Precautions
MediDrink Platinum is not suitable for:
- patients with galactosemia
- patients with hereditary fructose intolerance (fructosemia)
- children below 3 years of age
Packaging
MediDrink Platinum is available in 4 flavors: strawberry, chocolate, coffee, and vanilla.
MediDrink Platinum comes in liquid format in 200-ml Tetra Pak packaging in a ready-to-drink format, with a foil-wrapped plastic straw on each individual pack, or in 330-ml Tetra Prisma packaging with a plastic screw cap.
SAFETY OF LOW-CARBOHYDRATE-HIGH-FAT NUTRITION
Low-carbohydrate-high fat nutrition is safe (Hite et al. 2011, Ruth et al. 2013, Dehghan et al. 2017, Niswender et al. 2018). Low glycemic load nutrition is more beneficial for diabetic patients (Venn & Green. 2007, Fajcsák and Lelovics. 2006).
MediDrink Platinum is suitable also for elderly patients with diabetes (Medifood Data on file 2016).
Cardiovascular risk
Larosa et al. were the first to demonstrate in 1980 (and confirmed by others many times since) that low-carbohydrate diets (30-130 g/day) do not necessarily require higher fat or protein intakes, and a spontaneous decrease in overall calorie consumption frequently results in little protein or fat added back for the carbohydrate removed (Larosa et al. 1980). This causes the phenomenon that a very low carbohydrate diet ameliorates all the investigated anthropometric laboratory parameters (BMI, abdominal fat, triglycerides, HDL, triglycerides/HDL ratio, ApoB/ApoA1 ratio, small LDL, blood glucose, plasma insulin, saturated fatty acid) of patients with atherogenic dyslipidemia (Hite et al. 2011). In a study, which randomized obese subjects (29.0-44.6 kg/m2) recruited from Boston Medical Center to a hypocaloric low-fat-high-carbohydrate / LFHC (n=26) or high-fat-low-carbohydrate / HFLC (n=29) diet for 12 weeks, the HFLC group had greater improvements in blood lipids and systemic inflammation with similar changes in body weight and composition, relative to the LFHC group (Ruth et al. 2013).
Beneficial effects of a low-carbohydrate diet in obese subjects (Ruth et al. 2013)
In a large, epidemiological cohort study of individuals aged 35–70 years in 18 countries with a median follow-up of 7.4 years (IQR 5.3-9.3), dietary intake of 135,335 individuals was recorded using validated food frequency questionnaires. Participants were categorized into quintiles of nutrient intake (carbohydrate, fats, and protein) based on percentage of energy provided by nutrients. During follow-up, 5,796 deaths and 4,784 major cardiovascular disease events were documented. Higher carbohydrate intake was associated with an increased risk of total mortality (highest [quintile 5] vs lowest quintile [quintile 1] category, HR=1.28 [95% CI 1.12-1.46], ptrend=0.0001) but not with the risk of cardiovascular disease or cardiovascular disease mortality. Intake of total fat and each type of fat was associated with lower risk of total mortality (quintile 5 vs quintile 1, total fat: HR=0.77 [95% CI 0.67-0.87], ptrend<0.0001; saturated fat [SF], HR=0.86 [0.76-0.99], ptrend=0.0088; monounsaturated fat [MUFA]: HR=0.81 [95% CI 0.71-0.92], ptrend<0.0001; and polyunsaturated fat [PUFA]: HR=0.80 [95% CI 0.71-0.89], ptrend<0.0001). Higher saturated fat intake was associated with lower risk of stroke (quintile 5 vs quintile 1, HR=0.79 [95% CI 0.64-0.98], ptrend=0.0498). Total fat and saturated and unsaturated fats were not significantly associated with risk of myocardial infarction or cardiovascular disease mortality. Based on these results, the authors suggest the reconsideration of global dietary guidelines (Dehghan et al. 2017).
In a large, epidemiological cohort study, high carbohydrate intake was associated with higher risk of total mortality, whereas total fat and individual types of fat were related to lower total mortality (Dehghan et al. 2017).
One hundred and forty-four premenopausal women of age 21-50 years with class I/II obesity (BMI 30-39.9 kg/m2) were recruited in a study to keep a balanced high-fat diet (50% fat, 30% carbohydrate, 15% protein, with a balanced fat content – 1/3 saturated fatty acids, 1/3 monounsaturated fatty acids, 1/3 polyunsaturated fatty acids) for 16 weeks. To control the effects of high simple carbohydrate intake, total carbohydrate was maintained as 50% sugars (mono- and disaccharides) and 50% starches. Results in European American and African American participants were analyzed separately. Consuming the balanced high-fat diet significantly reduced cardiovascular risk by 5.5% (increased HDL particle size, increased the number of large HDL particle size, and increased apolipoprotein AI level) in both groups. In addition, European American women had significant reductions in fasting insulin levels (by 24.8%), and in HOMA-insulin resistance (by 29%). In the group of European American women, the most significant improvements occurred in VLDL particle size, apolipoprotein B levels, serum triglyceride, number of plasma LDL particles, and serum LDL cholesterol (Niswender et al. 2018).
High-fat balanced diet improves atherosclerotic cardiovascular disease risk in obese premenopausal women (Niswender et al. 2018)
Diabetes
The concept of glycemic load (GL) has been introduced by Walter Willett at the Harvard School of Public Health in 2004. While glycemic index (GI) ranks the different sources of carbohydrates according to their blood sugar-raising capacity, GL takes also into account the quantity of food / carbohydrates consumed. GL is calculated by multiplying the GI of the carbohydrates by the quantity of the carbohydrates taken in. Therefore, GL of a certain food depends not only on the GI but also the quantity consumed (Venn & Green 2007, Fajcsák & Lelovics. 2006). Based on the calculation of GL, MediDrink Platinum has the lowest GL and therefore the lowest strain on the metabolism of the patients among the different ONS depicted below. Thus, MediDrink Platinum is suitable also for malnourished elderlies with diabetes, since when consuming the same amounts of kilocalories, the GL of MediDrink Platinum is lower than that of the ONS specifically designed for diabetic patients.
MediDrink Platinum has the lowest strain on the metabolism of diabetic patients, since its glycemic load is lower than that of the diabetes-specific oral nutritional supplements
(Venn & Green. 2007, Fajcsák and Lelovics. 2006, Medifood Data on file 2016, http://www.nutricia.ie accessed on 19th October 2015, http://www.fresenius-kabi.co.uk accessed on 19th October 2015, http://www.fresenius-kabi.ie accessed on 19th October 2015, https://www.nestlehealthscience.com/brands/resource/resource-senioractiv accessed on 14th February 2020).
References
Allepaerts S. et al. [Nutrition in the elderly]. Rev Med Liege 2014;69:244-50.
Barberger-Gateau P. et al. Fish, meat, and risk of dementia: cohort study. Br Med J 2002;325:932-3.
Chentli F. et al. Diabetes mellitus in elderly. Indian J Endocrinol Metab 2015;19:744-52.
Fajcsák Zs. and Lelovics Zs. [Glycemic index and glycemic load]. Új Diéta 2006;4:28-9.
Hite AH. et al. Low-carbohydrate diet review: shifting the paradigm. Nutr Clin Pract 2011;26:300-8.
http://www.fresenius-kabi.co.uk accessed on 19th October 2015
http://www.fresenius-kabi.ie accessed on 19th October 2015
http://www.nutricia.ie accessed on 19th October 2015
https://www.nestlehealthscience.com/brands/resource/resource-senioractiv accessed on 14th February 2020
Medifood Data on file 2016.
Pirlich M et al. The German hospital malnutrition study. Clin Nutr 2006;25:563-72.
Richman EA. Geographic atrophy: an advanced from of dry AMD. 2008. Available at: http://www.eyesight2008.org/ accessed on 9th December 2023.
Salto3TM Quality Statements 2006
Shock MW. Human aging – Physiology and sociology. 2015. Accessed on 2nd February 2016
Yanai H. Nutrition for sarcopenia. J Clin Med Res 2015;7:926-31.
Zhang Y. and Jordan JM. Epidemiology of osteoarthritis. Clin Geriatr Med 2010;26:355-69.