Disease-related malnutrition
About disease-related malnutrition
Malnutrition or malnourishment is a condition that occurs if the body does not get the right amount of nutrients to maintain its health. When this is due to the effects of a disease or illness we call it disease-related malnutrition.
Therapeutic areas of disease-related malnutrition
- Cancers – Oncology
- Respiratory diseases – Pulmonology
- Stomach and intestinal diseases – Gastroenterology
- Age-related degenerative disorders – Elderly
There are 5 types of nutrients our body needs in order to function properly: carbohydrates, proteins, fats, vitamins and minerals. The sufficient quantities and the balance of these nutrients is essential to maintain our health. The body uses these nutrients to provide energy for growth, for healing and for any physical or mental exercise in general. When it does not get enough nutrients or not in the right balance, it becomes malnourished.
Disease-related malnutrition is the type of malnutrition that is triggered by illness or disease. It is the primary reason for malnutrition in developed countries, especially in the elderly since many of the diseases triggering malnutrition are related to age.
The most common diseases that can cause malnutrition include oncological diseases such as cancer, pulmonary diseases such as chronic obstructive pulmonary disease (COPD) or cystic fibrosis (CF) and gastroenterological diseases such as inflammatory bowel disease (IBD). Certain treatments of these diseases can also have a negative impact on nutrition, such as chemotherapy or radiation therapy.
Malnutrition is actually just as much a cause as a consequence of ill health: poor food intake, especially for a prolonged period, makes us more prone to illness and injury that can lead to a reduced appetite through a wide variety of mechanisms resulting in poor food intake. Thus, it is a vicious circle which often requires medical help to interrupt.
Disease-related malnutrition can develop for many reasons.
During illness patients tend to eat less than normal even though nutritional needs are higher as the body needs more energy to heal and recover. The loss of appetite generally comes down to several reasons. One of them might be the side-effects of treatment as different therapies or medicines may cause nausea and vomiting or require significant dietary restrictions. Depression could provide another reason for loss of appetite for it can make patients lose interest in food and eating in general. Pain can also be a cause because certain injuries make it painful to chew or to swallow.
Some patients have practical problems which prevent them from getting the right amount of nutrients, for instance preparing food and inserting it into the mouth in case of patients suffering from cachexia or Parkinson’s disease.
Another cause of malnutrition lies in gastrointestinal problems, in other words impaired function of the stomach and the small and large intestines. Disease can reduce the efficiency of digestion, so nutrients are not converted into a usable form. In other cases, nutrients may be expelled too soon for instance due to diarrhoea. Diseases including Crohn’s disease and ulcerative colitis may lead to such conditions
After an injury, trauma or surgery there is an extremely high demand for nutrients in the body to repair the essential organs or tissues that are damaged in addition to the body’s ordinary functions.
Thus, disease-related malnutrition comes down to 3 aspects which are interlinked: increased nutritional requirements (such as during an illness or after a trauma), reduced nutritional intake (due to pain, loss of interest or side-effects of treatment) and increased nutritional losses (due to malabsorption, vomiting or diarrhoea).
Source: http://www.dhsspsni.gov.uk/index/index-good-nutrition/gn-context/gn-disease-malnutrition.htm
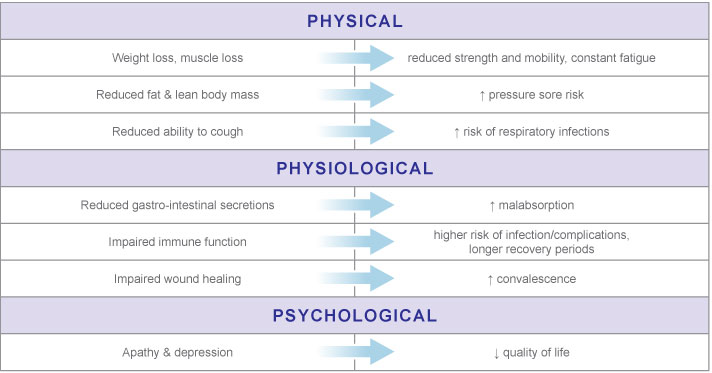
If the diet does not provide for increased nutritional demands, protein stores in the body are broken down to supply the required energy. This results in weight loss and a reduced quantity of muscles which in turn leads to physical weakness and vulnerability, thus the patients are more likely to fall and injure themselves. Because the immune system is also weakened, there is a greater chance of infection. Malnourished patients tend to experience frequent illnesses with longer recovery periods as their body is less resilient. Wound healing takes longer as well, and so the time of convalescence increases resulting in longer hospital stays. Malnourished patients often need to be re-admitted to a healthcare facility or require on-going healthcare services after being discharged from the hospital. They also tend to have a significantly higher number of total complications than well-nourished patients, for instance there is a higher risk of developing pneumonia and related mortality.
Sustained malnutrition may result in even more serious conditions, such as impaired functioning of the heart, lungs, and gastrointestinal system. Weakness might turn into cachexia, a severe condition marked by weight loss, muscle loss, and general weakness in a scale that prevents patients from performing tasks on their own and this from living an independent life.
In addition to all the physical and physiological consequences above, there are negative psychological consequences to consider. Insufficient nutritional intake leads to constant fatigue and it might result in apathy and even depression.
Shortly, to avoid all the above. Malnutrition has numerous negative consequences, resulting in a lower quality of life for patients.
Getting the right amount of nutrients is crucial for preventing weight loss and muscle wasting which helps keep up strength, overcome weakness and tiredness. It also helps keep the immune system healthy in order to avoid complications, infections, and, ultimately, to recover quicklier – regardless what disease the patients are fighting. Well-nourished patients are less likely to suffer from psychological consequences and so not only have a better prognosis but a better quality of life as well.
The main source of nutrients is normally food. However, for patients suffering from disease-related malnutrition, a healthy diet is often not enough. Since the nutritional demand is increased but appetite is reduced, patients need nutritional supplements that contain high energy in low volume, so even a little quantity boosts significantly the nutritional intake. Specially formulated nutritional products are available for patients to stay well-nourished and fight disease more effectively.
The condition-specific FSMP’s of Medifood is meant to meet these special nutritional needs. There are currently nine products available in our condition-specific portfolio addressing the special needs of the following conditions: cancer, chronic obstructive pulmonary disease, cystic fibrosis, inflammatory bowel disease, malnutrition in the case of elderly patients, as for surgical patients and and for patients with reduced glucose tolerance.